Keratoconus Treatment
Sub Title
Keratoconus (KC) is a condition that causes the cornea (the clear window in the front of the eye) to become thin, weak, and slowly sag over time. This change can cause progressive and substantial vision loss which may require eye surgery. KC typically starts in late childhood or the early teenage years and tends to be progressive. A variant of KC called Pellucid Marginal Degeneration tends to develop in adulthood and is less severe than typical KC. Estimates of the prevalence for keratoconus range from 1 in 500 to 1 in 2000 people. The exact cause of the disease is still be debated but there is a strong correlation between genetic, environmental, and hormonal factors. Eye rubbing is a preventable risk factor in the development of keratoconus. In rare circumstances, KC can also occur after LASIK surgery (called post-LASIK ectasia).
KC is typically treated in early stages with glasses and soft contact lenses because most patients have nearsighted astigmatism from the disease. As the disease progresses, scleral of gas-permeable lenses may be required for best vision. Surgical intervention may become necessary and end-stage KC may require corneal transplantation. The less invasive surgical techniques (described below) of corneal crosslinking (which can stop the progression of the disease) or Intacs (small plastic corneal inserts which can normalize corneal shape) may be indicated.
Keratoconus Treatment
Until recently there has been no treatment to slow or stop the progression of keratoconus.
– Paul Dougherty, MD
Medical Monitor
- EARLY STAGE – Glasses and toric soft contact lenses (corrects astigmatisms and nearsightedness). CXL can be used to prevent progression.
- MID STAGE – Scleral or Rigid Gas Permeable Contact Lenses (RGP’s). When traditional lenses cannot be used due to KC progression, Scleral or Specialty RGP’s may be sized for a proper fit to maintain adequate vision and comfort. CXL can be used to prevent progression.
- MID-LATE STAGE – Intacs corneal implants with or without corneal cross-linking. Used to reshape the cornea without removing corneal tissue and provide functional vision with the help of soft lenses/glasses.
- LATE STAGE – Partial or full-thickness corneal transplantation. The severely keratoconic and possibly scarred cornea is replaced with healthy donor corneal tissue sourced from a cadaver donor from a regional eye bank. Typically requires 12 to 18 months for visual rehabilitation before stabilizing and can last 10 to 15 years. Most patients still require a scleral or RGP contact lens to see well after the procedure.
Corneal Crosslinking (CXL)
Crosslinking Overview
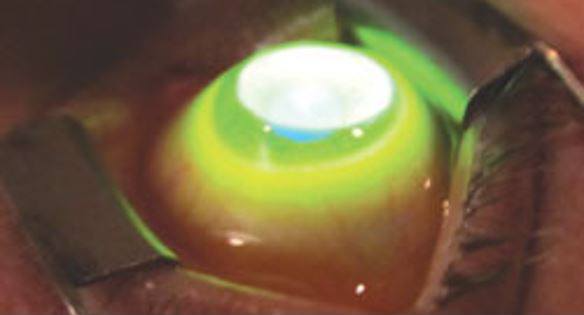
Corneal crosslinking (CXL) is a technique to prevent progression of keratoconus that utilizes Vitamin B (Riboflavin) drops placed onto the cornea and then exposing the cornea to ultraviolet (UV) light to stiffen the cornea by crosslinking the collagen fibrils responsible for corneal stability. The treatment is only performed to prevent progression of the disease, not to improve vision. You will still need to wear glasses or contacts lenses or have refractive surgery with Visian ICL or PRK to improve vision.
Traditional (CXL), which was first used over a decade ago, is performed by removing the surface cells (epithelium) of the eye (epi-off technique) which slows recovery time and increases the risk of infection. Epi-off CXL treatment was recently approved by the FDA. The downsides of epi-off CXL include pain, prolonged recovery time as the surface cells of the eye heal (up to 2 weeks of blurred vision and discomfort) and an increased risk of haze (scarring) or infection. At DLV, we typically only use epi-off CXL if the treatment is being done (off-label) to treat fluctuation in vision after Radial Keratotomy (RK) or if there is a significant progression of the disease after epi-on CXL (which we have never seen).
At DLV, we most commonly recommend epi-on CXL where the surface skin (epithelium) of the eye is left intact and a formulation of Vitamin B that penetrates the cornea through the epithelium is used. While not quite as effective as epi-off, there are many studies (including our own data) demonstrating the efficacy of the epi-on technique at preventing progression of keratoconus. The benefits of epi-on vs. epi-off CXL are vision recovery (24-48 hours vs. weeks), and much less risk of haze and infection than epi-off CXL. Typically, you may experience pain or discomfort after epi-on CXL for the first 12-24 hours, but you are typically comfortable and have functional vision by the next day.
Epi-on CXL is not specifically approved or disapproved by the FDA and is performed as an off-label procedure where your surgeon determines that a particular treatment is in your best interest. Epi-on CXL is commonly performed throughout the world.
Since the first large study was released in 2005 that showed that progress was halted in 100% of the 127 eyes involved, cross-linking has shown tremendous results worldwide.
Requirements for Treatment
- 12 Years of age or older
- Progressive keratoconus or other ectatic diseases
- Ectasia (LASIK-induced keratoconus)
- Fluctuating refraction after RK (+0.75D variation)
- Adequate corneal thickness (determined during your consultation)
- No or minimal corneal scarring
Intacs
Intacs overview
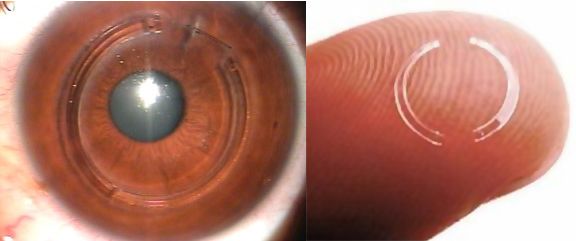
INTACS Inserts are two curved, clear plastic segments that are implanted in the perimeter of the cornea to reduce nearsightedness (myopia and astigmatism) in patients with keratoconus. The Inserts are implanted through a small surgical incision on the perimeter of the cornea created with a laser. The inserts help improve vision and contact lens fit in keratoconus patients by flattening and repositioning the cornea.
We perform Intacs less often than previously because of newer contact lenses for keratoconus such as scleral lenses that give better vision and are easier to fit than older contact lenses. We always prefer scleral or RGP lenses over Intacs because they allow for a better quality of vision, are safer and achieve more predictable outcomes than Intacs. After Intacs are implanted, patients will still be required to wear glasses or contacts to achieve the best vision.
INTACS Inserts are intended for patients with keratoconus who are no longer able to achieve adequate vision or fit/comfort using contact lenses or glasses or for patients who are considering vision corrective surgery with Visian ICL or PRK to get the best possible vision without glasses or contacts.

INDICATIONS FOR TREATMENT
- 12 years of age or older
- Progressive keratoconus or other ectatic diseases
- Post-LASIK (or other corneal refractive procedure) ectasia
- Poor vision or fit with scleral or RGP contact lenses
- KC patients who want better vision with glasses or soft contact lenses
- KC patients interested in improving their vision without glasses or contacts with surgery (Visian ICL or PRK)
- No central corneal scarring
- Adequate corneal thickness
